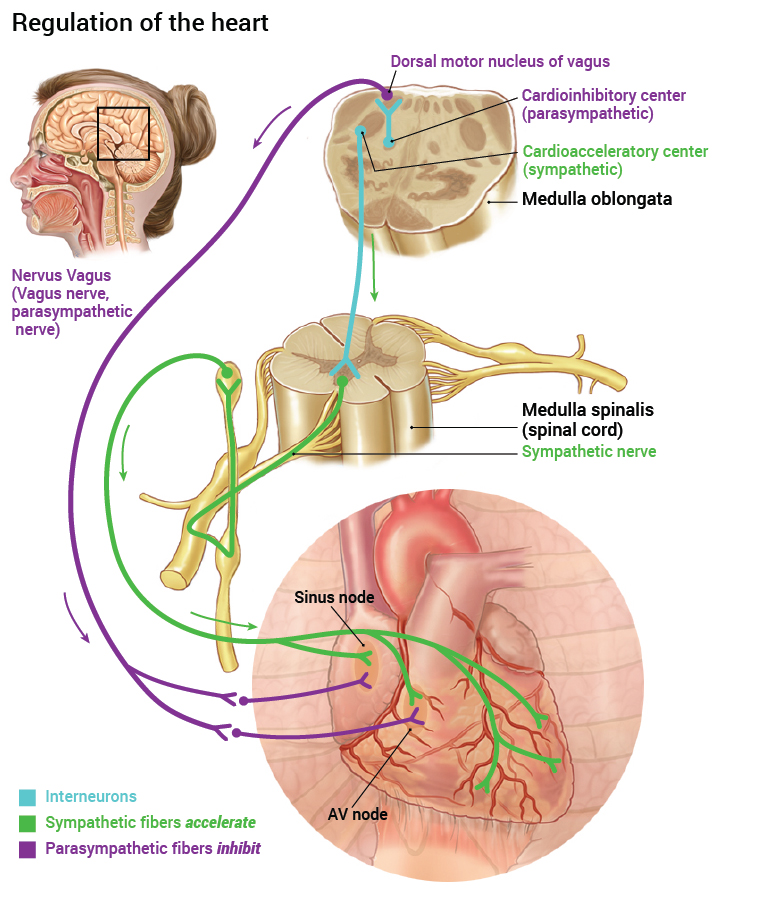
The heart’s contractions are not completely dependent on pacemaker cells. Contractions are regulated by the autonomic nervous system.
Parasympathetic nerves, the vagus nerve (cranial nerve X) arises from the medulla oblongata, and innervates the sinus node (and AV node). Here the nerve cells release the neurotransmitter substance acetylcholine. When acetylcholine binds its receptor, ion channels for K+ open. K+ then leaks out of the cells. This means that there must be more leakage of Na+ into these pacemaker cells to reach the threshold for spontaneous ion channel opening and depolarisation. Consequently it takes longer for the nerve impulse to be generated and the heart rate slows down.
Parasympathetic nerve stimulation lowers the heart rate. This explains why the sinus node depolarisation frequency is about 75-100 bpm but your resting heart rate is only 50-60 beats per minute.
Sympathetic nerve stimulation increases the depolarisation frequency of the heart. Sympathetic nerves are attached to the myocardium of the sinus node. The neurotransmitter substance from the sympathetic nerves is noradrenaline. Noradrenaline acts on β1 receptors in the heart and enables the threshold of the ion channels in the sinus node to be reached more quickly – thus increasing the depolarisation frequencies. In other words, the heart rate increases. In addition, sympathetic stimulation elsewhere in the myocardium promotes increased Ca2+ transport into the muscle cells. This provides increased muscle strength or power. This makes the heart able to contract both faster and more powerfully, and consequently the heart can squeeze out more blood per heartbeat.
During cardiac arrest patients may be treated with adrenaline, intravenously. Adrenaline mimics sympathetic activity, whereas atropine blocks the parasympathetic stimuli and is used in bradycardic arrhythmias (a slow abnormal rhythm) such as complete heart block to increase the heart rate. The effect is increased rate of contraction of the heart.